Braaaiiinnnnssss
2804
66
1

Welcome to Part 3 of neurology teaching! I am a neurology resident who loves teaching medical students, fellow residents, and my patients-- and one of my favorite ways to teach is using images.
Today I am taking a little departure from my usual pictures to talk about something that many are at least a little familiar with: Meningitis, or inflammation of the lining that surrounds the brain (the meninges).
There are a ton of things that can cause meningitis. I'm going to talk about meningococcal, pneumococcal and herpes meningitis.
(The picture above is a normal FDG-PET scan of the brain)
Part 1: https://imgur.com/gallery/DTKTFU1
Part 2: https://imgur.com/gallery/jzjpPoD
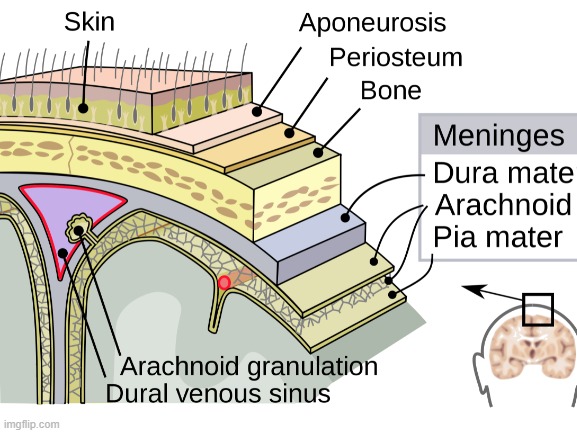
The meninges are a series of 3 layers that surround the brain, protecting it from the coarse bone of the skull, containing and reabsorbing cerebrospinal fluid (CSF), the fluid that bathes the brain, and supporting the structures of the many blood vessels which course inside the skull (among other important functions).
Unlike the brain itself, the meninges contain sensory receptors for pain, meaning irritation or inflammation of the meninges can be perceived by the brain as pain. The brain, on the other hand, does not contain sensory receptors for pain (as far as we know), but rather does the interpreting part of pain signals which go to the brain from elsewhere in the body.

When a patient comes into the hospital and we suspect bacterial meningitis (we'll get to this in a bit), we first make sure they're stable (breathing, OK blood pressure, etc), then we give antibiotics, antiviral and steroids (sometimes), and while we're making sure this gets done we get set up to do a lumbar puncture, also called a spinal tap.
It is important to not delay giving antibiotics in order to coordinate a lumbar puncture due to the high mortality rate of bacterial and herpes meningitis. We also almost always get a head CT to make sure there is no mass or large bleed in the head which would make a lumbar puncture unsafe. We also usually will get a set of labs to make sure the patient isn't at an increased risk for serious bleeding.
I do these procedures frequently and only on adults (so far). Usually the patient will lie on their side and curl up into the fetal position with minimal rotational displacement of the back. Using my hands I locate the iliac crests (hip bones), then follow an imaginary line at the iliac crests to the patient's spine. This is about the L3/4 level of the lumbar spine, which is well below the termination of the spinal cord. I then make an indentation with a pen cap in between the spinous processes to mark my spot. Next I make up my sterile field, numb the area and likely tract of my spinal needle with lots of lidocaine, then insert the spinal needle to get some CSF. CSF usually flows slowly, but the whole procedure typically takes 30 minutes.

CSF is made by the choroid plexus in the ventricles of the brain. It is supposed to be clear and colorless, with a relatively low amount of protein, essentially no cells, and a set amount of glucose (can be high with diabetes). There should be no red blood cells, white blood cells, or bacterial cells. There should also not be viral particles in the CSF.
The CSF tube on the left is normal in appearance. The next two are what is called xanthochromic, which is seen with small amounts of red blood cells in the CSF. Note the CSF is still clear, but more yellow. Blood in the CSF can be caused by hitting a small vessel or venous plexus during lumbar puncture (also called traumatic tap), can be caused by subarachnoid hemorrhage, or hemorrhagic meningitis/encephalitis. Tube 4 is not only bloody, but also cloudy. With enough blood from the above causes, you can get white blood cells and excess protein in the CSF which make it cloudy. Tube 5 is somewhat red as well but even more cloudy or turbid. This degree of cloudiness is suspicious for excessive white blood cells, as can be seen with infection or serious inflammation.
There are many diseases which can result in changes to CSF appearance, but I will focus on infectious meningitis.

Our first meningitis is Meningococcal meningitis. Caused by the bacteria Neisseria meningitidis. It can affect people with normal immune systems easily. Many strains of this infection are preventable by vaccination, so it is uncommon to see in the hospital systems in countries where this vaccine is widely available for all. In the US most people will get vaccinated in their teenage years.
Good thing a vaccine is available because it's contagious via respiratory droplets and if you are in close contact with someone with the disease you will often need antibiotic prophylaxis.
People unfortunate enough to get meningococcal meningitis, not only get the classic high fever, headache and neck stiffness, but also may be treated to a variety of terrifying complications, including severe myalgias, sore throat, profound fatigue or loss of consciousness, leg pain, petechial/purpuric rash, shock, disseminated intravascular coagulation (basically your blood excessively clots and bleeds too much at the same time), massive cutaneous hemorrhagic necrosis (purpura fulminans), seizures, myocarditis, and the list goes on. It is often fatal or severely disabling, particularly without prompt treatment.

Streptococcal meningitis is the most common cause of meningitis among adults in the US. There are thoughts that rates of this disease are declining among younger age groups at least in part due to campaigns to vaccinate older adults against S. pneumo (to prevent pneumonia).
It presents similarly to meningococcal meningitis, but does not have the dramatic skin findings, clotting/bleeding issues, or usually as severe of a systemic illness. People with this disease often have high fevers, headaches, stiff necks and alterations in mental status. They may also have seizures and focal neurologic deficits (weakness, sensory changes, face droop, difficulty speaking, etc)

Herpes causes inflammation of the brain (encephalitis) and also of the meninges. Within the careers of my slightly older colleagues this disease has gone from fatal > 70% of the time and disabling the rest of the time to fatal ~30% of the time with various degrees of disability for most survivors (few return back to their pre-infection baseline). This is a feared complication of herpes infection-- which could be new infection or latent infection. It is thankfully very uncommon (whereas herpes infection in general is practically ubiquitous). Inflammation of the brain is classically seen in the medial temporal lobes, which are the parts of the brain responsible for new memory formation. It is also a part of the brain that is susceptible to becoming a seizure focus when damaged. (The scan on the left has brighter signal in the medial temporal lobe, indicating inflammation)
People that get herpes encephalitis often are very, very sick. They have headaches, fevers, often stiff necks like other meningitides. They also frequently have seizures, memory impairments, alterations in consciousness and focal neurologic deficits (due to the direct infection of the brain).
Diagnosis is made via PCR (polymerase chain reaction) from the CSF.
Treatment is IV acyclovir at very high doses for several weeks. Delays of even a few hours in treatment are associated with worse outcomes.

How do we treat meningitis? In theory we could tailor our anti-infective approach based on clinical suspicion and culture data, but in reality when we have someone we're worried about bacterial or herpes meningitis in we usually take more of a kitchen-sink approach due to the high mortality rate if untreated. Cultures and PCR take time to come back, time the patient in front of you does not have. You can always stop medications when certain infections are ruled out.
For most folks age 2-50, the most likely culprits in bacterial meningitis are Neisseria meningitidis and Streptococcus pneumoniae. In this age group we treat empirically with vancomycin and ceftriaxone, 2 common antibiotics. If they're over 50 we add in ampicillin to cover Listeria monocytogenes and aerobic gram negative bacilli.
If bacterial meningitis is suspected we will give steroids as well (dexamethasone) prior to or with the antibiotics in order to reduce neurologic complications seen with Strep. pneumoniae infections. If evaluation for S. pneumo is negative, we will stop the steroid.
Until we get CSF results, we also usually will give IV acyclovir as well to treat possible herpes meningitis.

Thanks for reading and letting me share my love of neurology with you!
Stay tuned for future posts :)
Lostarchitorture
Had contracted meningitis @6 weeks old. The symptoms or long term effects from it are still noticeable with me today at 40+ years old
danielm2100
Interesting post! Will continue to follow
trippingthelightfantastic
Wow! Great post @OP. Thank you.
salunatics
Zimyoumoron
Thanks @op. +1 and favorited. I had meningitis as a kid so reading about it was pretty cool.
Braaaiiinnnnssss
Glad you liked it! There is a lot of variability in individual experiences, but this is just my clinical experience
insaneinthehalfbrain
Cool informative post! Wish it was a bit simplified cause I am just a common person.
DrDizzo
I am so thankful to you for posting this. I just recovered from Meningitis about 2 months ago. An absolutely horrible experience! Good info!
Braaaiiinnnnssss
I'm glad you're on the road to recovery! Happy to provide some information from the neurology perspective :)
MissDeeMeanor
Avoid swimming in fresh water lakes, especially small ones.
Braaaiiinnnnssss
This is to avoid Naegleria fowleri (sp?)-- cerebral amebiasis. Very rare. Usually in areas that don't freeze.